Primary Biliary Cirrhosis
What is primary biliary cirrhosis?
Primary biliary cirrhosis is a chronic, or long lasting, disease that causes the small bile ducts in the liver to become inflamed and damaged and ultimately disappear.
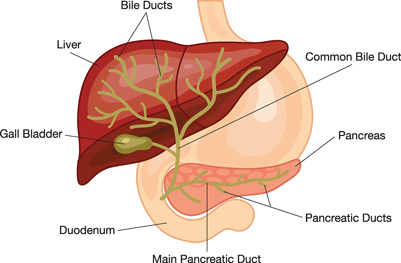
The bile ducts carry a fluid called bile from the liver to the gallbladder, where it is stored. When food enters the stomach after a meal, the gallbladder contracts, and the bile ducts carry bile to the duodenum, the first part of the small intestine, for use in digestion. The liver makes bile, which is made up of bile acids, cholesterol, fats, and fluids. Bile helps the body absorb fats, cholesterol, and fat-soluble vitamins. Bile also carries cholesterol, toxins, and waste products to the intestines, where the body removes them. When chronic inflammation, or swelling, damages the bile ducts, bile and toxic wastes build up in the liver, damaging liver tissue.
This damage to the liver tissue can lead to cirrhosis, a condition in which the liver slowly deteriorates and is unable to function normally. In cirrhosis, scar tissue replaces healthy liver tissue, partially blocking the flow of blood through the liver.
The liver is the body’s largest internal organ. The liver is called the body’s metabolic factory because of the important role it plays in metabolism—the way cells change food into energy after food is digested and absorbed into the blood. The liver has many functions, including
- taking up, storing, and processing nutrients from food—including fat, sugar, and protein—and delivering them to the rest of the body when needed
- making new proteins, such as clotting factors and immune factors
- producing bile
- removing waste products the kidneys cannot remove, such as fats, cholesterol, toxins, and medications
A healthy liver is necessary for survival. The liver can regenerate most of its own cells when they become damaged. However, if injury to the liver is too severe or long lasting, regeneration is incomplete, and the liver creates scar tissue. Scarring of the liver may lead to cirrhosis.

By BruceBlaus (Own work) [CC BY-SA 4.0], via Wikimedia Commons
The buildup of scar tissue that causes cirrhosis is usually a slow and gradual process. In the early stages of cirrhosis, the liver continues to function. However, as cirrhosis gets worse and scar tissue replaces more healthy tissue, the liver will begin to fail. Chronic liver failure, which is also called end-stage liver disease, progresses over months, years, or even decades. With end-stage liver disease, the liver can no longer perform important functions or effectively replace damaged cells.
Primary biliary cirrhosis usually occurs between the ages of 30 and 65 and affects women more often than men.1
1
[Top]
What causes primary biliary cirrhosis?
The causes of primary biliary cirrhosis are unknown. Most research suggests it is an autoimmune disease. The immune system protects people from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances. An autoimmune disease is a disorder in which the body’s immune system attacks the body’s own cells and organs. In primary biliary cirrhosis, the immune system attacks the small bile ducts in the liver.
Genetics, or inherited genes, can make a person more likely to develop primary biliary cirrhosis. Primary biliary cirrhosis is more common in people who have a parent or sibling—particularly an identical twin—with the disease. In people who are genetically more likely to develop primary biliary cirrhosis, environmental factors may trigger or worsen the disease, including
- exposure to toxic chemicals
- smoking
- infections
Genetics can also make some people more likely to develop other autoimmune diseases, such as
- autoimmune hepatitis, a disease in which the body’s immune system attacks liver cells
- Sjögren’s syndrome, a condition in which the immune system attacks the glands that produce tears and saliva
- autoimmune thyroid dysfunctions, conditions in which the immune system attacks the thyroid gland
[Top]
What are the symptoms of primary biliary cirrhosis?
The first and most common symptoms of primary biliary cirrhosis are
- fatigue, or feeling tired
- itching skin, and darkened skin in itching areas due to scratching
- dry eyes and mouth
Some people may have jaundice, a condition that causes the skin and whites of the eyes to turn yellow. Health care providers diagnose up to 60 percent of people with primary biliary cirrhosis before symptoms begin.2 Routine blood tests showing abnormal liver enzyme levels may lead a health care provider to suspect that a person without symptoms has primary biliary cirrhosis.
2
[Top]
What are the complications of primary biliary cirrhosis?
Most complications of primary biliary cirrhosis are related to cirrhosis and start after primary biliary cirrhosis progresses to cirrhosis. In some cases, portal hypertension and esophageal varices may develop before cirrhosis.
Portal hypertension. The portal vein carries blood from the stomach, intestines, spleen, gallbladder, and pancreas to the liver. In cirrhosis, scar tissue partially blocks the normal flow of blood, which increases the pressure in the portal vein. This condition is called portal hypertension. Portal hypertension is a common complication of cirrhosis. This condition may lead to other complications, such as
- edema—swelling due to a buildup of fluid—in the feet, ankles, or legs, and ascites—a buildup of fluid in the abdomen
- enlarged blood vessels, called varices, in the esophagus, stomach, or both
- an enlarged spleen, called splenomegaly
- mental confusion due to a buildup of toxins that are ordinarily removed by the liver, a condition called hepatic encephalopathy
Edema and ascites. Liver failure causes fluid buildup that results in edema and ascites. Ascites can lead to spontaneous bacterial peritonitis, a serious infection that requires immediate medical attention.
Varices. Portal hypertension may cause enlarged blood vessels in the esophagus, stomach, or both. These enlarged blood vessels, called esophageal or gastric varices, cause the vessel walls to become thin and blood pressure to increase, making the blood vessels more likely to burst. If they burst, serious bleeding can occur in the esophagus or upper stomach, requiring immediate medical attention.
Splenomegaly. Portal hypertension may cause the spleen to enlarge and retain white blood cells and platelets, reducing the numbers of these cells and platelets in the blood. A low platelet count may be the first evidence that a person has developed cirrhosis.
Hepatic encephalopathy. A failing liver cannot remove toxins from the blood, so they eventually accumulate in the brain. The buildup of toxins in the brain is called hepatic encephalopathy. This condition can decrease mental function and cause stupor and even coma. Stupor is an unconscious, sleeplike state from which a person can only be aroused briefly by a strong stimulus, such as a sharp pain. Coma is an unconscious, sleeplike state from which a person cannot be aroused. Signs of decreased mental function include
- confusion
- personality changes
- memory loss
- trouble concentrating
- a change in sleep habits
Metabolic bone diseases. Some people with cirrhosis develop a metabolic bone disease, which is a disorder of bone strength usually caused by abnormalities of vitamin D, bone mass, bone structure, or minerals, such as calcium and phosphorous. Osteopenia is a condition in which the bones become less dense, making them weaker. When bone loss becomes more severe, the condition is referred to as osteoporosis. People with these conditions are more likely to develop bone fractures.
Gallstones and bile duct stones. If cirrhosis prevents bile from flowing freely to and from the gallbladder, the bile hardens into gallstones. Symptoms of gallstones include abdominal pain and recurrent bacterial cholangitis—irritated or infected bile ducts. Stones may also form in and block the bile ducts, causing pain, jaundice, and bacterial cholangitis.
Steatorrhea. Steatorrhea is a condition in which the body cannot absorb fat, causing a buildup of fat in the stool and loose, greasy, and foul-smelling bowel movements. Steatorrhea may be caused by impairment of bile delivery to the small intestine or by the pancreas not producing enough digestive enzymes.
Liver cancer. Liver cancer is common in people with cirrhosis. Liver cancer has a high mortality rate. Current treatments are limited and only fully successful if a health care provider detects the cancer early, before the tumor is too large. For this reason, health care providers should check people with cirrhosis for signs of liver cancer every 6 to 12 months. Health care providers use blood tests, ultrasound, or both to check for signs of liver cancer.
[Top]
How is primary biliary cirrhosis diagnosed?
A health care provider may use the following tests to diagnose primary biliary cirrhosis:
- a medical and family history
- a physical exam
- blood tests
- imaging tests
- a liver biopsy
A health care provider usually bases a diagnosis of primary biliary cirrhosis on two out of three of the following criteria:
- a blood test showing elevated liver enzymes
- a blood test showing the presence of anti-mitochondrial antibodies (AMA)
- a liver biopsy showing signs of the disease
Health care providers may order additional tests to rule out other causes of symptoms. Health care providers diagnose the majority of people with primary biliary cirrhosis early in the course of the disease.
Medical and family history. Taking a medical and family history is one of the first things a health care provider may do to help diagnose primary biliary cirrhosis. He or she will ask a patient to provide a medical and family history.
Physical exam. A physical exam may help diagnose primary biliary cirrhosis. During a physical exam, a health care provider usually
- examines a patient’s body
- uses a stethoscope to listen to sounds in the abdomen
- taps on specific areas of the patient’s body
The health care provider will perform a physical exam to look for signs of the disease. For example, the liver may feel hard or ascites may cause the abdomen to enlarge.
Blood test. A blood test involves drawing blood at a health care provider’s office or a commercial facility and sending the sample to a lab for analysis. The blood test can show elevated levels of liver enzymes, such as alkaline phosphatase. A routine blood test may show high levels of the liver enzyme alkaline phosphatase in people who have primary biliary cirrhosis and are not yet showing symptoms.
The health care provider will perform an AMA blood test to help confirm the diagnosis. A blood test will detect the presence of AMA in 90 to 95 percent of people with primary biliary cirrhosis.3
Imaging tests. A health care provider may use the following imaging tests to examine the bile ducts. These tests can distinguish between primary biliary cirrhosis and other conditions that affect the bile ducts.
- Ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. A specially trained technician performs the procedure in a health care provider’s office, an outpatient center, or a hospital, and a radiologist—a doctor who specializes in medical imaging— interprets the images. A patient does not need anesthesia. In addition to showing problems with the bile ducts, the images can show signs of advanced cirrhosis or complications.
- Magnetic resonance cholangiopancreatography uses magnetic resonance imaging (MRI) to examine the bile ducts. MRI machines use radio waves and magnets to produce detailed pictures of the body’s internal organs and soft tissues without using x rays. A specially trained technician performs magnetic resonance cholangiopancreatography in an outpatient center or a hospital, and a radiologist interprets the images. A patient does not need anesthesia, though a health care provider may use light sedation for patients with a fear of confined spaces. With most MRI machines, the patient lies on a table that slides into a tunnel-shaped device that may be open ended or closed at one end; some machines allow the patient to lie in a more open space.
- Endoscopic retrograde cholangiopancreatography uses an x ray to look at the bile ducts. A gastroenterologist—a doctor who specializes in digestive diseases—performs the test at a hospital or an outpatient center. After lightly sedating the patient, the gastroenterologist inserts an endoscope—a small, flexible tube with a light and a camera on the end—through the mouth into the duodenum and bile ducts. The endoscope is connected to a computer and video monitor. The gastroenterologist injects a special dye, called contrast medium, through the tube into the bile ducts, which makes the ducts show up on the monitor. This test is more invasive than other imaging tests, and health care providers do not routinely need the test to make the diagnosis of primary biliary cirrhosis. A health care provider uses the test selectively when he or she is concerned that the blockage of the bile ducts has another cause, such as a gallstone or a narrowing of the large bile ducts due to inflammation or cancer. Patients may have pain, nausea, or vomiting after the test or may develop bacterial cholangitis or pancreatitis—inflammation of the pancreas.
Liver biopsy. A liver biopsy is a procedure that involves taking a piece of liver tissue for examination with a microscope for signs of damage or disease. The health care provider may ask the patient to stop taking certain medications temporarily before the liver biopsy. The health care provider may ask the patient to fast for 8 hours before the procedure.
During the procedure, the patient lies on a table, right hand resting above the head. The health care provider applies a local anesthetic to the area where he or she will insert the biopsy needle. If needed, a health care provider will also give sedatives and pain medication. The health care provider uses a needle to take a small piece of liver tissue. He or she may use ultrasound, computerized tomography scans, or other imaging techniques to guide the needle. After the biopsy, the patient must lie on the right side for up to 2 hours and is monitored an additional 2 to 4 hours before being sent home.
A health care provider performs a liver biopsy at a hospital or an outpatient center. The health care provider sends the liver sample to a pathology lab, where the pathologist—a doctor who specializes in diagnosing diseases—looks at the tissue with a microscope and sends a report to the patient’s health care provider.
A liver biopsy can confirm the diagnosis of primary biliary cirrhosis; however, a person does not always need this test. A health care provider will perform a biopsy if the AMA blood test is negative and the person shows other signs of primary biliary cirrhosis. Sometimes a health care provider finds a cause of liver damage other than primary biliary cirrhosis during biopsy.

3
[Top]
How is primary biliary cirrhosis treated?
Treatment for primary biliary cirrhosis depends on how early a health care provider diagnoses the disease and whether complications are present. In the early stages of primary biliary cirrhosis, treatment can slow the progression of liver damage to cirrhosis. In the early stages of cirrhosis, the goals of treatment are to slow the progression of tissue scarring in the liver and prevent complications. As cirrhosis progresses, a person may need additional treatments and hospitalization to manage complications.
Medications
Health care providers prescribe ursodiol (Actigall, Urso) to treat primary biliary cirrhosis. Ursodiol is a nontoxic bile acid that people can take orally. Ursodiol replaces the bile acids that are normally produced by the liver, which are more toxic and can harm the liver. Treatment with ursodiol can reduce levels of bilirubin and liver enzymes in the blood. Early treatment with this medication reduces the likelihood of needing a liver transplant and improves survival.3 Early treatment provides the most benefit; however, ursodiol treatment late in the course of the disease can still slow the progression of liver damage. While ursodiol treatment improves the outcome of primary biliary cirrhosis, it does not cure the disease.
Researchers are studying the effects of several other medications on the progression of primary biliary cirrhosis. To date, none has shown the positive effects of ursodiol.
Avoiding Alcohol and Other Substances
People with cirrhosis should not drink any alcohol or take any illegal substances, as both will cause more liver damage. People with cirrhosis should avoid complementary and alternative medications, such as herbs. People with cirrhosis should be careful about starting new medications and should consult a health care provider before taking prescription medications, over-the-counter medications, or vitamins. Many vitamins and prescription and over-the-counter medications can affect liver function.
Treatment of Symptoms and Complications
Health care providers treat symptoms and complications as follows:
Itching. Antihistamines may help with mild itching. However, antihistamines often cause drowsiness, and a person should take antihistamines just before bedtime to help with nighttime itching. A health care provider will treat more problematic itching with cholestyramine (Locholest, Questran), which reduces cholesterol in the blood. Experts believe high levels of cholesterol let substances that cause itching build up in tissues.
Dry eyes and mouth. Health care providers usually treat dry eyes and mouth with artificial tears and saliva substitutes, respectively. These products are available without a prescription. A health care provider may treat people whose symptoms do not improve with pilocarpine (Salagen) or cevimeline (Evoxac). People who have difficulty with dry eyes should see an ophthalmologist—a doctor who diagnoses and treats all eye diseases and eye disorders—regularly. People with dry mouth should have regular dental exams.
Portal hypertension. A health care provider may prescribe a beta-blocker or nitrate to treat portal hypertension. Beta-blockers lower blood pressure by helping the heart beat slower and with less force, and nitrates relax and widen blood vessels to let more blood flow to the heart and reduce the heart’s workload.
Varices. Beta-blockers can lower the pressure in varices and reduce the likelihood of bleeding. Bleeding in the stomach or esophagus requires an immediate upper endoscopy. This procedure involves using an endoscope to look for varices. The health care provider may use the endoscope to perform a band ligation, a procedure that involves placing a special rubber band around the varices that causes the tissue to die and fall off. A gastroenterologist performs the procedure at a hospital or an outpatient center. People who have had varices in the past may need to take medication to prevent future episodes.
Edema and ascites. Health care providers prescribe diuretics—medications that remove fluid from the body—to treat edema and ascites. A health care provider may remove large amounts of ascitic fluid from the abdomen and check for spontaneous bacterial peritonitis. A health care provider may prescribe bacteria-fighting medications called antibiotics to prevent infection. He or she may prescribe oral antibiotics; however, severe infection with ascites requires intravenous (IV) antibiotics.
Hepatic encephalopathy. A health care provider will treat hepatic encephalopathy by cleansing the bowel with lactulose, a laxative given orally or as an enema—a liquid put into the rectum. A health care provider may also add antibiotics to the treatment. Hepatic encephalopathy may improve as other complications of cirrhosis are controlled.
Osteoporosis. A health care provider may prescribe bisphosphonate medications to improve bone density.
Gallstones and bile duct stones. A health care provider may use surgery to remove gallstones. He or she may use endoscopic retrograde cholangiopancreatography, which uses balloons and basketlike devices, to retrieve the bile duct stones.
Liver cancer. A health care provider may recommend screening tests every 6 to 12 months to check for signs of liver cancer. Screening tests can find cancer before the person has symptoms of the disease. Cancer treatment is usually more effective when the health care provider finds the disease early. Health care providers use blood tests, ultrasound, or both to screen for liver cancer in people with cirrhosis. He or she may treat cancer with a combination of surgery, radiation, and chemotherapy.
[Top]
When is a liver transplant considered for primary biliary cirrhosis?
A health care provider may consider a liver transplant when cirrhosis leads to liver failure or treatment for complications is ineffective. Liver transplantation is surgery to remove a diseased or an injured liver and replace it with a healthy liver or part of a liver from another person, called a donor.
More information is provided in the NIDDK health topic, Liver Transplantation.
[Top]
Eating, Diet, and Nutrition
A healthy diet is important in all stages of cirrhosis because malnutrition is common in people with this disease. Malnutrition is a condition that occurs when the body does not get enough nutrients. Cirrhosis may lead to malnutrition because it can cause
- people to eat less because of symptoms such as loss of appetite
- changes in metabolism
- reduced absorption of vitamins and minerals
Health care providers can recommend a meal plan that is well balanced and provides enough calories and protein. If ascites develops, a health care provider or dietitian may recommend a sodium-restricted diet. To improve nutrition, the health care provider may prescribe a liquid supplement. A person may take the liquid by mouth or through a nasogastric tube—a tiny tube inserted through the nose and throat that reaches into the stomach.
A person with cirrhosis should not eat raw shellfish, which can contain a bacterium that causes serious infection. Cirrhosis affects the immune system, making people with cirrhosis more likely than healthy people to develop an infection after eating shellfish that contain this bacterium.
A health care provider may recommend calcium and vitamin D supplements to help prevent osteoporosis.
[Top]
Points to Remember
- Primary biliary cirrhosis is a chronic disease that causes the small bile ducts in the liver to become inflamed and damaged and ultimately disappear.
- When chronic inflammation damages the bile ducts, bile and toxic wastes build up in the liver, damaging liver tissue. This damage to the liver tissue can lead to cirrhosis.
- The causes of primary biliary cirrhosis are unknown. Most research suggests it is an autoimmune disease.
- Primary biliary cirrhosis is more common in people who have a parent or sibling—particularly an identical twin—with the disease.
- The first and most common symptoms of primary biliary cirrhosis are fatigue, itching, and dry eyes and mouth. Some people may have jaundice, a condition that causes the skin and whites of the eyes to turn yellow. Health care providers diagnose up to 60 percent of people with primary biliary cirrhosis before symptoms begin.
- Most complications of primary biliary cirrhosis are related to cirrhosis and start after primary biliary cirrhosis progresses to cirrhosis.
- A health care provider may use the following tests to diagnose primary biliary cirrhosis:
- a medical and family history
- a physical exam
- blood tests
- imaging tests
- a liver biopsy
- Health care providers prescribe ursodiol (Actigall, Urso) to treat primary biliary cirrhosis. Early treatment with this medication reduces the likelihood of needing a liver transplant and improves survival.
- A health care provider may consider a liver transplant when cirrhosis leads to liver failure or treatment for complications is ineffective.
[Top]
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for youExternal NIH Link.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.govExternal Link Disclaimer.
This information may contain content about medications and, when taken as prescribed, the conditions they treat. When prepared, this content included the most current information available. For updates or for questions about any medications, contact the U.S. Food and Drug Administration toll-free at 1-888-INFO-FDA (1-888-463-6332) or visit www.fda.govExternal Link Disclaimer. Consult your health care provider for more information.
The U.S. Government does not endorse or favor any specific commercial product or company. Trade, proprietary, or company names appearing in this document are used only because they are considered necessary in the context of the information provided. If a product is not mentioned, the omission does not mean or imply that the product is unsatisfactory.
[Top]
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. The NIDDK translates and disseminates research findings through its clearinghouses and education programs to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by the NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
M. Eric Gershwin, M.D., University of California; Gregory Gores, M.D., and Jayant A. Talwalkar, M.D., M.P.H., both from the Mayo Clinic
This information is not copyrighted. The NIDDK encourages people to share this content freely.
[Top]
April 2014
